Medical Insurance Claims Processing with AI: A European Success Story
In today’s fast-paced healthcare environment, the traditional insurance claims process often creates friction points that frustrate both patients and providers. Long processing times, communication gaps, and manual documentation requirements can delay critical care decisions and reimbursements.
KNOWLEDGEBOT
10/26/20242 min read


The Challenge: Modernizing Insurance Claims Management
In today’s fast-paced healthcare environment, the traditional insurance claims process often creates friction points that frustrate both patients and providers. Long processing times, communication gaps, and manual documentation requirements can delay critical care decisions and reimbursements. When a leading European medical insurance provider approached us with these challenges, we knew AI could transform their claims management landscape.
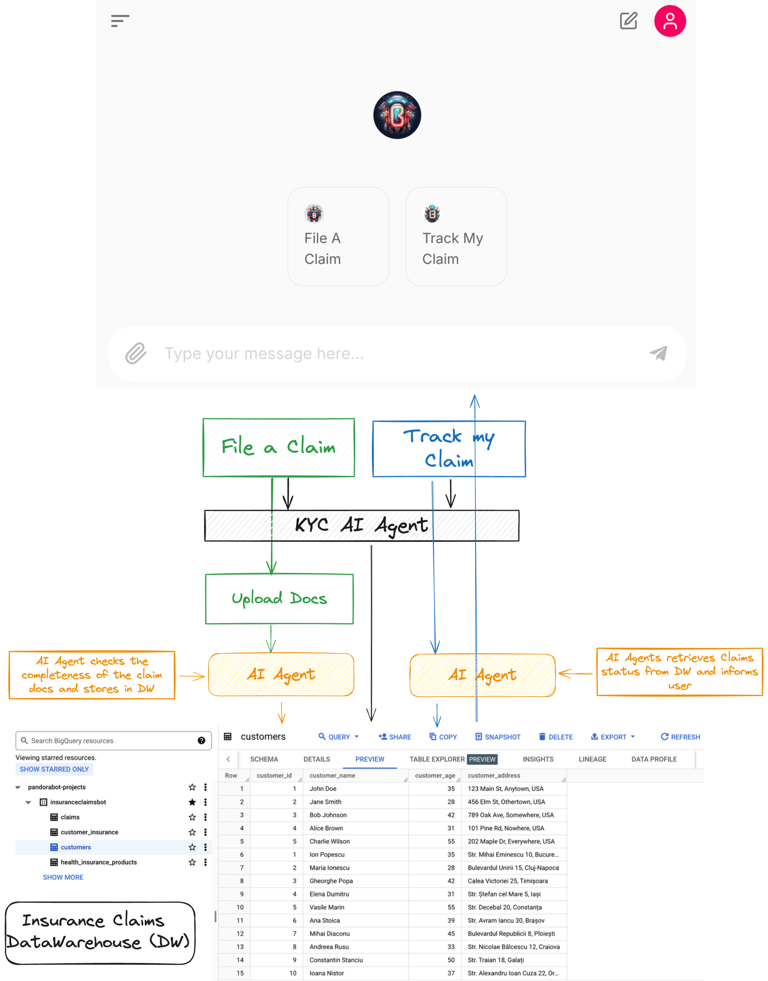
Enter PandoraBot’s Insurance Claims Bot
Our solution? A sophisticated AI-powered claims bot that streamlines the entire claims process, from initial filing to final resolution. Here’s how it works:
1. Seamless Authentication & Verification
Secure customer verification through contract numbers and personal identifiers
Integration with existing customer databases for real-time validation
Multi-language support for diverse European customer base
2. Intelligent Document Processing
Advanced computer vision capabilities for processing medical receipts and documentation
Automatic extraction of critical information (claim amounts, procedures, dates)
Real-time validation against policy terms and coverage limits
3. Smart Claims Management
Automated claim status tracking and updates
Instant response to customer queries about claims status
Integration with backend systems for seamless data flow
The Impact: Numbers Tell the Story
The implementation has delivered impressive results:
70% reduction in claims processing time
24/7 availability for claim submissions and status checks
85% reduction in manual document handling
90% customer satisfaction with the claims process
Significant cost savings in claims processing operations
Key Features That Made the Difference
Multimodal Intelligence
The bot’s ability to process both text and images means customers can simply snap photos of their medical receipts and documentation. The AI automatically extracts relevant information, eliminating manual data entry and reducing errors.
Real-Time Processing
Rather than waiting days for claims to be processed, customers receive immediate feedback on their submissions. The system can instantly verify:
Policy coverage
Document completeness
Claim validity
Expected processing time
Natural Language Understanding
The bot handles customer queries in natural language, making it accessible to users regardless of their technical expertise. Whether asking about claim status, coverage details, or required documentation, customers receive clear, contextual responses.
The Human Touch: AI-Assisted, Not AI-Replaced
While the bot handles routine tasks and inquiries automatically, it’s designed to seamlessly escalate complex cases to human agents. This hybrid approach ensures:
Complex claims receive appropriate attention
Special circumstances are handled with care
Customer satisfaction remains high
Compliance with regulatory requirements
Looking Ahead: The Future of Insurance Claims
This successful implementation points to a future where AI transforms insurance claims processing from a bureaucratic burden into a smooth, efficient experience. We envision:
Predictive analytics for fraud detection
Automated policy recommendations based on claim patterns
Enhanced integration with healthcare provider systems
Expanded multilingual capabilities
Conclusion: A Win for All Stakeholders
The success of this implementation demonstrates that AI-powered solutions can deliver tangible benefits to insurers and customers alike. By combining cutting-edge technology with deep industry knowledge, we’ve created a system that:
Speeds up claims processing
Reduces operational costs
Improves customer satisfaction
Frees up human agents for value-added tasks
The insurance industry is ripe for AI-driven transformation, and this deployment shows what’s possible when innovation meets practical needs. As we continue to refine and enhance our solutions, we’re excited about the potential to bring similar transformations to insurance providers worldwide.
Want to learn how AI can transform your insurance operations? Visit PandoraBot.io to schedule a demo and see our insurance claims bot in action.